AI Predicts Cardiovascular Disease Before Patient Becomes Aware of Underlying Condition
|
By HospiMedica International staff writers Posted on 24 Jan 2022 |
For the first time ever, scientists have shown that artificial intelligence (AI) could lead to better ways to predict the onset and course of cardiovascular disease.
A new AI-based system developed by scientists at University of Utah Health (Salt Lake City, Utah, USA) mines Electronic Health Records (EHRs) and assesses the combined effects of various risk factors to better predict the onset and outcomes of heart disease. The researchers developed unique computational tools to precisely measure the synergistic effects of existing medical conditions on the heart and blood vessels.
The researchers say this comprehensive approach could help physicians foresee, prevent, or treat serious heart problems, perhaps even before a patient is aware of the underlying condition. Although the study only focused on cardiovascular disease, the researchers believe it could have far broader implications. In fact, they suggest that these findings could eventually lead to a new era of personalized, preventive medicine. Doctors would proactively contact patients to alert them to potential ailments and what can be done to alleviate the problem.
Current methods for calculating the combined effects of various risk factors - such as demographics and medical history - on cardiovascular disease are often imprecise and subjective. As a result, these methods fail to identify certain interactions that could have profound effects on the health of the heart and blood vessels. To more accurately measure how these interactions, also known as comorbidities, influence health, the researchers used machine learning software to sort through more than 1.6 million EHRs after names and other identifying information were deleted.
These electronic records, which document everything that happens to a patient, including lab tests, diagnoses, medication usage, and medical procedures, helped the researchers identify the comorbidities most likely to aggravate a particular medical condition such as cardiovascular disease. In their current study, the researchers used a form of AI called probabilistic graphical networks (PGM) to calculate how any combination of these comorbidities could influence the risks associated with heart transplants, congenital heart disease, or sinoatrial node dysfunction (SND, a disruption or failure of the heart’s natural pacemaker).
Among adults, the researchers found that individuals who had a prior diagnosis of cardiomyopathy (disease of the heart muscle) were at 86 times higher risk of needing a heart transplant than those who didn’t. They also found that those who had viral myocarditis had about a 60 times higher risk of requiring a heart transplant. In addition the usage of milrinone, a vasodilating drug used to treat heart failure, pushed the transplant risk 175 times. This was the strongest individual predictor of heart transplant. In some instances, the combined risk was even greater. For instance, among patients who had cardiomyopathy and were taking milrinone, the risk of needing a heart transplant was 405 times higher than it was for those whose hearts were healthier.
Comorbidities had a significantly different influence on the transplant risk among children, according to the researchers. Overall, the risk of pediatric heart transplant ranged from 17 to 102 times higher than children who didn’t have pre-existing heart conditions, depending on the underlying diagnosis. The researchers also examined influences that a mother’s health during pregnancy had on her children. Women who had high blood pressure during pregnancy were about twice as likely to give birth to infants who had congenital heart and circulatory problems. Children with Down syndrome had about three times greater risk of having a heart anomaly. Infants who had Fontan surgery, a procedure that corrects a congenital blood flow defect in the heart, were about 20 times more likely to develop SND heart rate dysfunction than those who didn’t need the surgery. The researchers also detected important demographic differences. For instance, a Hispanic patient with atrial fibrillation (rapid heartbeat) had twice the risk of SND compared with Blacks and Whites, who had similar medical histories.
“We can turn to AI to help refine the risk for virtually every medical diagnosis,” said Martin Tristani-Firouzi, M.D. the study’s corresponding author and a pediatric cardiologist at U of U Health. “The risk of cancer, the risk of thyroid surgery, the risk of diabetes—any medical term you can imagine.”
“This novel technology demonstrates that we can estimate the risk for medical complications with precision and can even determine medicines that are better for individual patients,” said Josh Bonkowsky, M.D. Ph.D., Director of the Primary Children’s Center for Personalized Medicine, who believes this research could lead to development of a practical clinical tool for patient care.
Related Links:
University of Utah Health
Latest Patient Care News
- First-Of-Its-Kind Portable Germicidal Light Technology Disinfects High-Touch Clinical Surfaces in Seconds
- Surgical Capacity Optimization Solution Helps Hospitals Boost OR Utilization

- Game-Changing Innovation in Surgical Instrument Sterilization Significantly Improves OR Throughput
- Next Gen ICU Bed to Help Address Complex Critical Care Needs
- Groundbreaking AI-Powered UV-C Disinfection Technology Redefines Infection Control Landscape
- Clean Hospitals Can Reduce Antibiotic Resistance, Save Lives
- Smart Hospital Beds Improve Accuracy of Medical Diagnosis
- New Fast Endoscope Drying System Improves Productivity and Traceability
- World’s First Automated Endoscope Cleaner Fights Antimicrobial Resistance
- Portable High-Capacity Digital Stretcher Scales Provide Precision Weighing for Patients in ER
- Portable Clinical Scale with Remote Indicator Allows for Flexible Patient Weighing Use
- Innovative and Highly Customizable Medical Carts Offer Unlimited Configuration Possibilities
- Biomolecular Wound Healing Film Adheres to Sensitive Tissue and Releases Active Ingredients
- Wearable Health Tech Could Measure Gases Released From Skin to Monitor Metabolic Diseases
- Wearable Cardioverter Defibrillator System Protects Patients at Risk of Sudden Cardiac Arrest
- World's First AI-Ready Infrasound Stethoscope Listens to Bodily Sounds Not Audible to Human Ear
Channels
Artificial Intelligence
view channel
AI-Powered Algorithm to Revolutionize Detection of Atrial Fibrillation
Atrial fibrillation (AFib), a condition characterized by an irregular and often rapid heart rate, is linked to increased risks of stroke and heart failure. This is because the irregular heartbeat in AFib... Read more
AI Diagnostic Tool Accurately Detects Valvular Disorders Often Missed by Doctors
Doctors generally use stethoscopes to listen for the characteristic lub-dub sounds made by heart valves opening and closing. They also listen for less prominent sounds that indicate problems with these valves.... Read moreCritical Care
view channel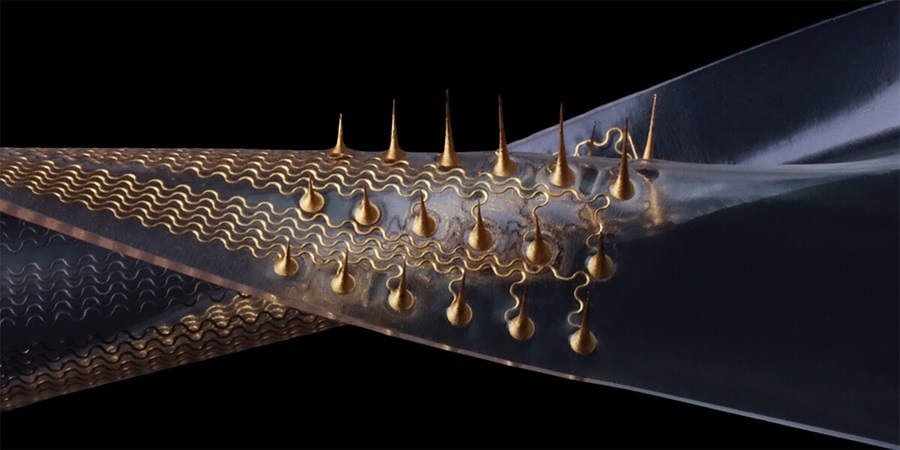
Stretchable Microneedles to Help In Accurate Tracking of Abnormalities and Identifying Rapid Treatment
The field of personalized medicine is transforming rapidly, with advancements like wearable devices and home testing kits making it increasingly easy to monitor a wide range of health metrics, from heart... Read more
Machine Learning Tool Identifies Rare, Undiagnosed Immune Disorders from Patient EHRs
Patients suffering from rare diseases often endure extensive delays in receiving accurate diagnoses and treatments, which can lead to unnecessary tests, worsening health, psychological strain, and significant... Read more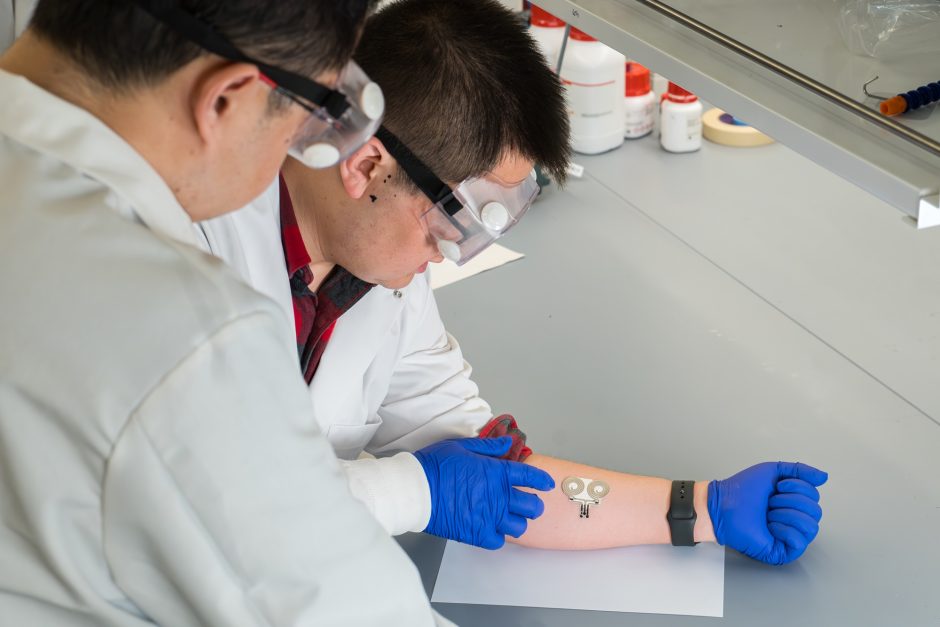
On-Skin Wearable Bioelectronic Device Paves Way for Intelligent Implants
A team of researchers at the University of Missouri (Columbia, MO, USA) has achieved a milestone in developing a state-of-the-art on-skin wearable bioelectronic device. This development comes from a lab... Read more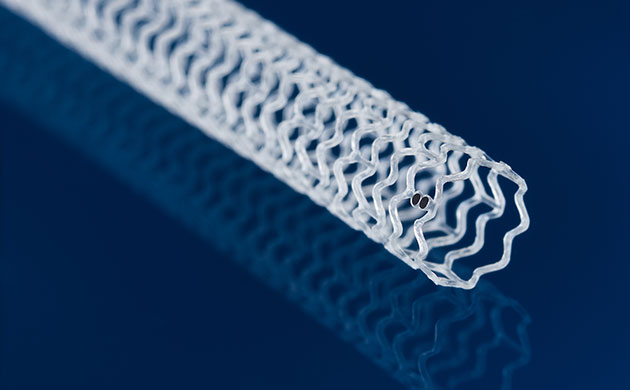
First-Of-Its-Kind Dissolvable Stent to Improve Outcomes for Patients with Severe PAD
Peripheral artery disease (PAD) affects millions and presents serious health risks, particularly its severe form, chronic limb-threatening ischemia (CLTI). CLTI develops when arteries are blocked by plaque,... Read moreSurgical Techniques
view channel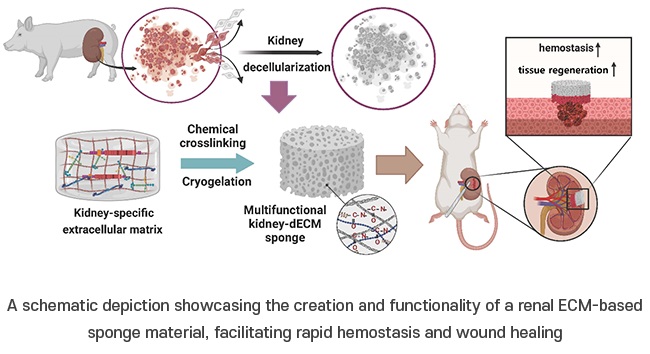
Porous Gel Sponge Facilitates Rapid Hemostasis and Wound Healing
The kidneys are essential organs that handle critical bodily functions, including waste elimination and blood pressure regulation. Often referred to as the silent organ because they typically do not manifest... Read more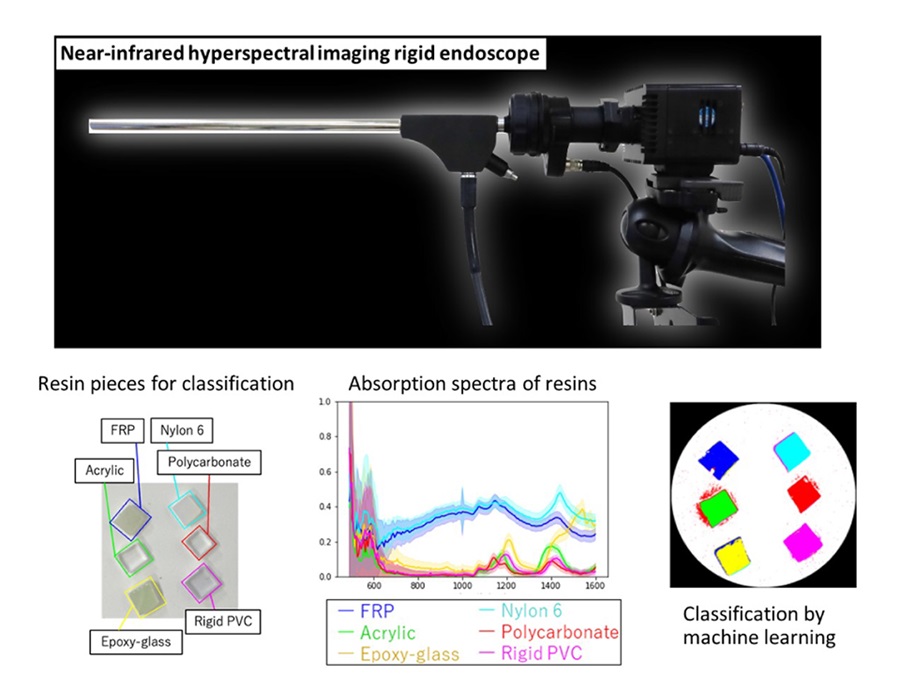
Novel Rigid Endoscope System Enables Deep Tissue Imaging During Surgery
Hyperspectral imaging (HSI) is an advanced technique that captures and processes information across a given electromagnetic spectrum. Near-infrared hyperspectral imaging (NIR-HSI) has particularly gained... Read more
Robotic Nerve ‘Cuffs’ Could Treat Various Neurological Conditions
Electric nerve implants serve dual functions: they can either stimulate or block signals in specific nerves. For example, they may alleviate pain by inhibiting pain signals or restore movement in paralyzed... Read more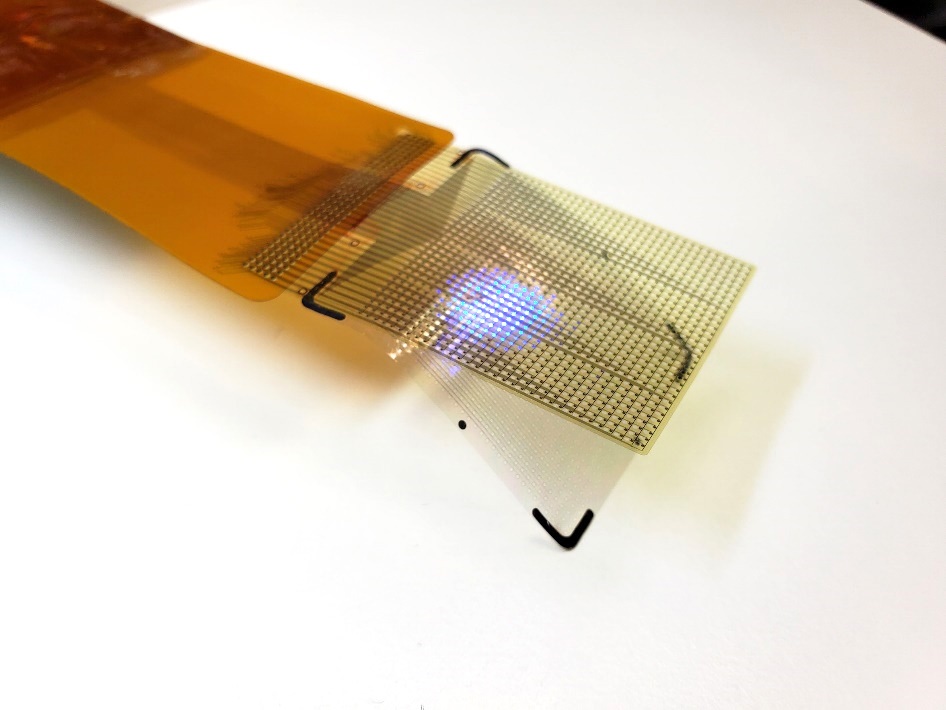
Flexible Microdisplay Visualizes Brain Activity in Real-Time To Guide Neurosurgeons
During brain surgery, neurosurgeons need to identify and preserve regions responsible for critical functions while removing harmful tissue. Traditionally, neurosurgeons rely on a team of electrophysiologists,... Read moreHealth IT
view channel
Machine Learning Model Improves Mortality Risk Prediction for Cardiac Surgery Patients
Machine learning algorithms have been deployed to create predictive models in various medical fields, with some demonstrating improved outcomes compared to their standard-of-care counterparts.... Read more
Strategic Collaboration to Develop and Integrate Generative AI into Healthcare
Top industry experts have underscored the immediate requirement for healthcare systems and hospitals to respond to severe cost and margin pressures. Close to half of U.S. hospitals ended 2022 in the red... Read more
AI-Enabled Operating Rooms Solution Helps Hospitals Maximize Utilization and Unlock Capacity
For healthcare organizations, optimizing operating room (OR) utilization during prime time hours is a complex challenge. Surgeons and clinics face difficulties in finding available slots for booking cases,... Read more
AI Predicts Pancreatic Cancer Three Years before Diagnosis from Patients’ Medical Records
Screening for common cancers like breast, cervix, and prostate cancer relies on relatively simple and highly effective techniques, such as mammograms, Pap smears, and blood tests. These methods have revolutionized... Read morePoint of Care
view channel
Critical Bleeding Management System to Help Hospitals Further Standardize Viscoelastic Testing
Surgical procedures are often accompanied by significant blood loss and the subsequent high likelihood of the need for allogeneic blood transfusions. These transfusions, while critical, are linked to various... Read more
Point of Care HIV Test Enables Early Infection Diagnosis for Infants
Early diagnosis and initiation of treatment are crucial for the survival of infants infected with HIV (human immunodeficiency virus). Without treatment, approximately 50% of infants who acquire HIV during... Read more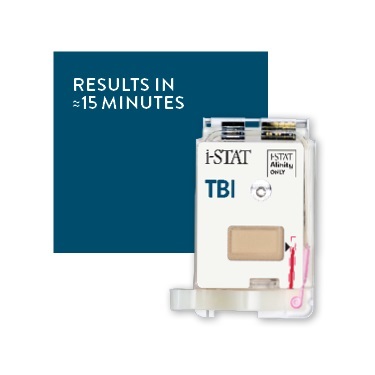
Whole Blood Rapid Test Aids Assessment of Concussion at Patient's Bedside
In the United States annually, approximately five million individuals seek emergency department care for traumatic brain injuries (TBIs), yet over half of those suspecting a concussion may never get it checked.... Read more
New Generation Glucose Hospital Meter System Ensures Accurate, Interference-Free and Safe Use
A new generation glucose hospital meter system now comes with several features that make hospital glucose testing easier and more secure while continuing to offer accuracy, freedom from interference, and... Read moreBusiness
view channel
Johnson & Johnson Acquires Cardiovascular Medical Device Company Shockwave Medical
Johnson & Johnson (New Brunswick, N.J., USA) and Shockwave Medical (Santa Clara, CA, USA) have entered into a definitive agreement under which Johnson & Johnson will acquire all of Shockwave’s... Read more